Cancer, Medicine and Life
A cancer and medicine blog to help on the journey of life. Medicine and Medical Oncology are rapidly changing fields and is hard for most people to keep up. A diagnosis of any illness, in particular cancer is devastating news for anyone, and the hope is that we can share knowledge and support each other.
Monday, 7 October 2019
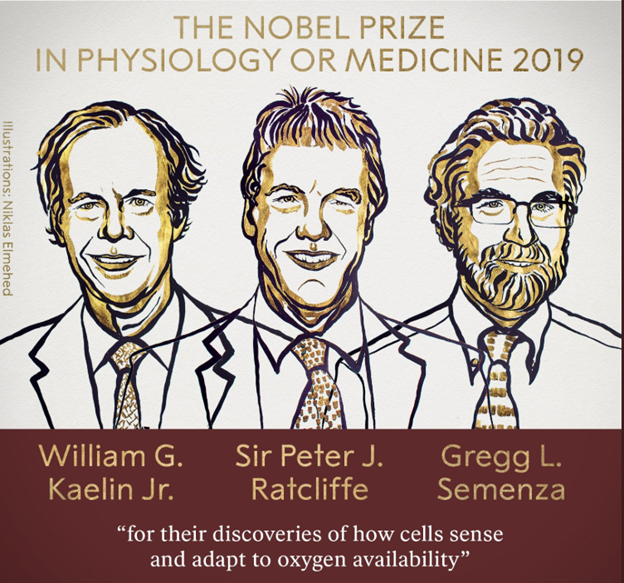
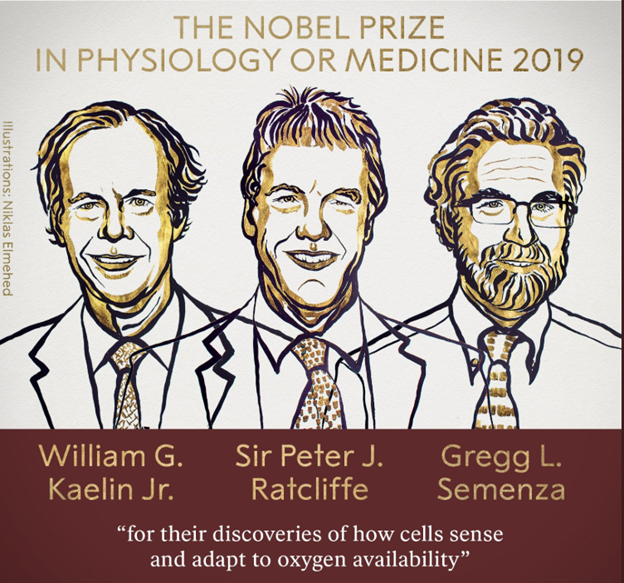
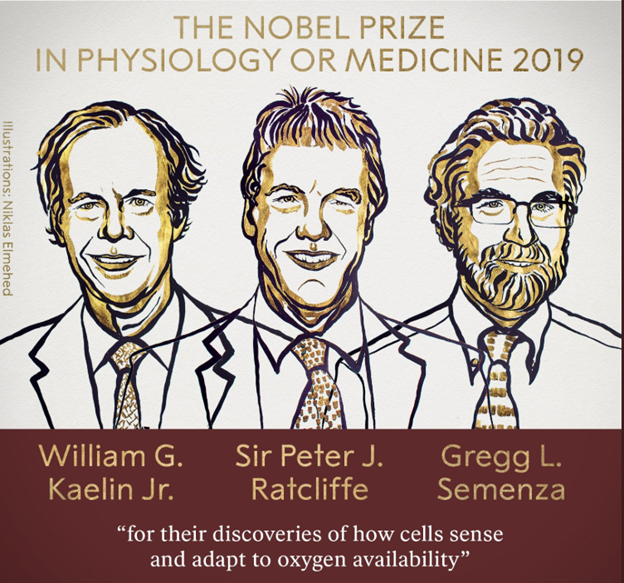
Nobel Prize in Medicine: 2019
The 2019 in Medicine has been awarded to William Kaelin Jr, Peter Ratcliffe and Gregg Semenza “for their discoveries of how cells sense and adapt to oxygen availability.” HIF1-alpha is at the center of this process, plays a key role in many cancers.
Saturday, 29 September 2018
Cost of "last wishes"
What is the cost of a patient's last wishes?
Most of us try our best to help complete the last wishes of our patients. Some near impossible, some just plain crazy and most possible with lots of help.
I will highlight some stories that I have collected over the years for patients. Will write about them over the next few days.
Most of us try our best to help complete the last wishes of our patients. Some near impossible, some just plain crazy and most possible with lots of help.
I will highlight some stories that I have collected over the years for patients. Will write about them over the next few days.
Monday, 12 March 2018
Tumours and Transformations
Text taken from The New England Journal of Medicine: http://www.nejm.org/doi/full/10.1056/NEJMp1716548?query=featured_hematology-oncology
Dr Scott Winner, MD
It happened 21 years ago, near the end of a night on-call. Around 5 a.m., the emergency department physician paged radiology and requested an ultrasound on a 41-year-old male with right upper quadrant pain. I walked down the hall and entered the exam room. A man lay on his back on a gurney and a woman leaned on the bed’s railing. An ultrasound machine and a small black stool were beside the bed. I introduced myself.
“I’m Dr. Winner. I’ll be doing your ultrasound. Where’s your pain, sir?”
“Right here.” He pointed below his right ribs.
“Okay. Let’s get started.”
I shut the door and flipped off the lights; the room darkened. As our eyes adjusted, I said to the woman, “So are you his better half?” Her lips turned up slightly and she nodded yes. I pulled up the patient’s shirt exposing his abdomen.
“How long have you two been married?”
“Nine years,” the man replied.
I squirted acoustic gel on his skin. He arched his back and said, “Whoa! That’s cold.”
“Sorry about that. I should’ve warned you.”
He sneered at me. I changed the subject.
“So, do you have kids?”
The patient turned his head toward his wife. She stared at him. I regretted asking. The patient looked back at me and said, “Our 2-year-old son died 2 weeks ago.”
“Oh…I’m sorry.”
The woman folded her arms on her chest.
“What, uh, what did your son die of?”
“He had cancer of the liver. Hepatoblastoma.”
For a moment, the three of us sat together, silent and breathing. The only sound in the room was the low hum of the machine.
I leaned forward, picked up the ultrasound probe and placed it on his belly. Bowel gas and blood vessels flashed on the screen. I moved the probe in search of his liver and said, “Okay, sir, take a deep breath in and hold it.” He did so, and his liver came into view. My breath stopped. For a few seconds, I just stared, then I angled the probe up, down, right, and left. The husband and wife were watching me.
She asked, “Do you see something?”
“You can breathe, sir.” He exhaled, and I pulled the probe off his skin. The screen went blank. Gazing at the machine, I said, “I’m just getting started.”
I fidgeted with the machine settings for no particular reason. I shifted in my seat. I placed the probe back on his skin and studied his kidneys, spleen, pancreas, aorta, and gallbladder. All were normal. I moved the probe back to his liver. There were masses everywhere. I measured some of the lesions and saved the images. I did not talk or look at the man or woman as I worked. I couldn’t. I knew something intimate and heartbreaking. This patient had just watched his child die of a liver tumor. And all the while, they had been dying together — father and son.
I put the probe down and covered the man’s skin with a clean, white towel.
“I’m finished.”
“What did you see?” the patient asked.
“Sir, you have, uh, your liver has lesions in it.”
“Is my gallbladder okay? They thought it was my gallbladder in the emergency room.”
“Your gallbladder is normal. You have liver masses.”
“You mean like cancer? You think I have cancer in my liver?”
“We’ll need to get a biopsy to prove it, but yes, sir, I do. I’m sorry.”
The woman reached between the bed rail bars and touched her husband’s bare waist with the back of her hand. I asked them if they had any questions, but neither answered. I stood up, paused, and left the room. The orderly was waiting in the hallway; I told him the patient was ready for transport. I called the emergency department doctor and gave her the results of the study. I went back into the hallway and saw the man being wheeled away, his wife’s silhouette walking behind. They turned a corner and disappeared.
My shift ended, and the morning crew arrived. One of my physician colleagues asked me about my night. My patient’s ultrasound films were still hanging on the viewbox in front of us. I showed him the images of the patient’s liver masses and started to tell him about the couple’s 2-year-old son, but my voice cracked. My colleague gently placed his hand on the nape of my neck. We stood there, shoulder to shoulder.
I left the hospital and drove home. I undressed and stepped into a hot shower. I put my head under the water and let it soak my scalp. When I closed my eyes, I saw vivid images of the father’s tumor-laden liver.
I was raised to believe that hard work and effort could solve any problem. The Little Engine That Could was my favorite childhood book, and I internalized the book’s mantra — “I think I can.” I was never the smartest kid in class, and it took me two attempts to get accepted to medical school. When I graduated and earned my M.D., my father gave me a framed quote by Calvin Coolidge, which read in part, “Persistence and determination alone are omnipotent. The slogan ‘press on’ has solved and always will solve the problems of the human race.” My response to setbacks and suffering was to try harder, to work harder. I did not know how to pray or meditate. On the Sunday mornings of my youth, my mother went to the Presbyterian church on West Water Street while my father and I slept in.
Prior to that night on call, I had seen many sad cases, among them a teenager shot in the head, an orthopedic surgeon sitting and sobbing next to his sick child, and a fetus dead in the womb. To cope, I occupied my time and mind with exercise, work, and tasks while the sadness of these cases dissolved somewhere inside. But for the father and son with cancer, there was no room, no space within me.
In the days following my experience with the patient, I tried to persist and press on, but I had entered an unknown world, one that I did not understand. My long-held beliefs and ways of being seemed inadequate. I went for a run but found myself walking and ruminating. I lost interest in studying medicine. After reading my 3-year-old daughter a book at bedtime, I stayed with her until the cadence and sound of her breath assured me that she was safely asleep.
A week after that night on call, a week after my center of gravity shifted, I am at work thinking about the father with cancer. I check the medical record for the pathology report of his liver biopsy. The result: adenocarcinoma. My gut aches. I notice that he is an inpatient in room 221. I think about visiting the patient, although I have no earthly reason to do so. There is no procedure to perform, no note to write, and no checklist to complete. But this is an impulse, one that I don’t understand and can’t ignore. I take off my white coat and hang it on a chair. I walk to the stairwell and climb. Looking down, I notice depressions on the surface of each step from all those who walked this path before me.
I arrive on the second floor, walk by the nurse’s station, and enter the hallway. Human voices rise and fade away as I travel. I’m searching for something. I find the patient’s room, and my pace slows. The door is open, and I enter his room. A few steps past the threshold, I stop. The physical world fades and thoughts fall away. What I encounter is ancient, transcendent, fearful, beautiful. The patient rests in bed. Family, friends, and the chaplain surround him. They all hold hands, heads bowed.
Treating his own Heart Attack!! - Only in Australia
Text taken from The New England Journal of Medicine: http://www.nejm.org/doi/full/10.1056/NEJMc1716701?query=featured_home
A 44-year-old man presented with severe chest pain and dizziness to the nursing post where he worked in Coral Bay, Australia, more than 1000 km from Perth and 150 km from the next nearest medical facility. He was the only nurse on duty when the symptoms occurred. Since no other medical personnel were available, he performed and emailed his own electrocardiograms to an emergency physician by means of the Emergency Telehealth Service (ETS). The first electrocardiogram showed complete heart block, right bundle-branch block, hyperacute T waves in the inferior leads, and reciprocal ST-segment depression in the anterolateral leads. The second electrocardiogram, obtained 50 minutes later, showed sinus tachycardia with 2 mm of inferior ST-segment elevation.
He self-cannulated both antecubital fossae for intravenous access and self-administered aspirin, clopidogrel, sublingual nitroglycerin, intravenous heparin, and opiates. Preparations were made for thrombolysis with tenecteplase, with real-time video interaction with the ETS. He attached his own defibrillator pads and prepared adrenaline, atropine, and amiodarone. After thrombolysis, there was resolution of his ST-segment elevation and symptoms.
He was transferred by the Royal Flying Doctor Service to a tertiary cardiology unit in Perth. The next day, coronary angiography revealed severe stenosis in the mid–right coronary artery with blood flow of Thrombolysis in Myocardial Infarction (TIMI) grade 3 and mild left ventricular systolic dysfunction. A drug-eluting stent was inserted, and his residual moderate coronary artery disease was managed medically. He was discharged home 48 hours later and continued appropriate medical therapy.
Western Australia covers more than 2.5 million square kilometers,1 and much of the state is sparsely populated. The provision of health care to persons living in rural locations is an ongoing challenge. In 2012, the Western Australian Department of Health started the ETS to provide health services to isolated communities, using health care professionals who could be accessed by means of information and communication technology.2 This system was intended to facilitate diagnosis and treatment and to aid in disease prevention, research, and continued education in these communities.3,4 The initiation of this service has improved the delivery and accessibility of health care.1
Thrombolysis is the standard treatment for patients with ST-segment elevation myocardial infarction who are more than 120 minutes away from a hospital that is capable of performing primary percutaneous coronary intervention.5 Patients undergoing thrombolysis also undergo cardiac monitoring, intravenous access, and monitoring for infarct-related and thrombolysis-related complications. In the absence of other trained medical personnel or resources, the actions of this patient are likely to have had a substantial beneficial effect on the clinical outcome. However, a person’s self-management of a myocardial infarction cannot be considered medically appropriate if any other option is available.
Felicity Lee, M.B., B.S.
Paul Maggiore, M.B., B.S.
Kevin Chung, M.B., B.S.
Sir Charles Gairdner Hospital, Nedlands, WA, Australia
Paul Maggiore, M.B., B.S.
Kevin Chung, M.B., B.S.
Sir Charles Gairdner Hospital, Nedlands, WA, Australia
References:
- 1. Dillon E, Loermans J, Davis D, Xu C. Evaluation of the Western Australian Department of Health telehealth project. J Telemed Telecare 2005;11:Suppl 2:S19-S21.
- 2. Herrington G, Zardins Y, Hamilton A. A pilot trial of emergency telemedicine in regional Western Australia. J Telemed Telecare 2013;19:430-433.
- 3. Bradford N, Caffery L, Smith A. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health 2016;16:3808-3808.
- 4. A health telematics policy in support of WHO’S Health-For-All Strategy for Global Development: report of the WHO Group Consultation on Health Telematics 11–16 December, Geneva, 1997. Geneva: World Health Organization, 1998(http://apps.who.int/iris/bitstream/10665/63857/1/WHO_DGO_98.1.pdf).
- 5. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127(4):e362-425.
Who to blame in a medical tragedy? (ABC)
The text is from the ABC website - http://www.abc.net.au/news/health/2018-02-15/dr-bawa-garba-who-is-to-blame-when-a-medical-tragedy-occurs/9417166
In 2011, Jack Adcock — a six-year-old boy with Down's syndrome, a congenital heart disease and heart failure — was admitted to Leicester Royal Infirmary in the United Kingdom.
He'd been sick overnight, with diarrhoea and vomiting. His breathing was shallow and he looked unwell.
The registrar on duty in the emergency paediatrics ward that day was Dr Hadiza Bawa-Garba.
Her consultant, (senior doctor) Dr Stephen O'Riordan, was teaching in another town that morning and Dr Bawa-Garba was doing the work of at least one other paediatric registrar, who was on leave. So Dr Bawa-Garba was covering various wards of the hospital, including maternity, taking calls from GPs, and dealing with other emergencies.
It was also her first day on duty for emergencies involving sick children, in an unfamiliar hospital and having recently returned from 14 months of maternity leave.
It was mid-morning when Dr Bawa-Garba first saw Jack Adcock. She put him on intravenous fluids and ordered blood tests and a chest X-ray.
One blood test showed his blood was too acidic — a sign of severe illness — but that improved later in the morning after Jack was given fluids.
It was another two hours before Jack's chest X-ray was done, and it took Dr Bawa-Garba longer to see it — but once she did, she realised the boy had pneumonia and that was the cause of his illness.
What she did not realise, and what no-one else realised, was that the infection had caused Jack to go into septic shock — he was having trouble maintaining enough output from the heart to stay alive.
Dr Bawa-Garba prescribed Jack antibiotics for his pneumonia, but he didn't get them for another hour. Around this time, the doctor's consultant returned to the hospital. He saw Jack's blood test results but didn't see the child.
Jack was already on a drug called enalapril for his heart condition. This drug takes the stress off the heart and lowers blood pressure and therefore shouldn't be used when someone is in shock.
Dr Bawa-Garba knew this, and deliberately didn't write him up for the drug. But despite there being no continuing prescription for it, someone later gave Jack enalapril — and he went into cardiac arrest.
When she arrived at the resuscitation she mistook Jack for another child in the ward who had a 'do-not-resuscitate' order on his notes and called off the resuscitation.
Another junior doctor present corrected the misunderstanding and efforts were resumed a minute later but they failed to revive Jack. He died less than 12 hours after being admitted to the hospital.
Mistakes made: But who's to blame?
Dr Bawa-Garba was convicted of manslaughter on the grounds of gross negligence in November 2015. She was then suspended from practice for 12 months by an independent tribunal.
But Britain's regulator of doctors, the General Medical Council, appealed that decision. They wanted her permanently struck off the medical register, arguing the doctor failed to act on signs Jack was seriously ill and therefore contributed to his death.
Last month the High Court of England and Wales found in favour of the GMC and struck off Dr Bawa-Garba for life.
In its decision, the High Court found that the tribunal had failed to adequately sanction Dr Bawa-Garba — given that a jury had decided her conduct was "truly exceptionally bad".
"This misconduct by manslaughter by gross negligence involved a particularly serious departure from the principles of "Good Medical Practice," and the behaviour was fundamentally incompatible with being a doctor," Justice Ouseley wrote in his High Court decision.
Among the failings of Dr Bawa-Garba listed by the court were that she ignored key signs Jack was critically ill (like the high amount of acid and lactate in his blood, warning signs of septic shock) and didn't raise concerns about Jack's health with the consultant when he arrived at the hospital about 4:30pm.
But the ruling sparked outcry from doctors in Britain and around the world, who say the case reflects systemic failures at the hospital and in the broader healthcare system, and that it could have happened to any one of them.
"I've worked for 10 years in the UK, including some of the most intensive hospital environments in the UK, and I've never faced a day such as reported as her having faced that day," said Dr Moosa Qureshi, a haematology trainee and cancer researcher at the University of Cambridge.
"The situation she was in was a situation which really was going to produce mistakes, and it wasn't only herself who was making those mistakes, though most of the blame seems to have been pinned on her."
Dr Qureshi is one of three doctors calling themselves 'Team Hadiza' — they've fundraised over 300,000 pounds ($530,000) to pay for legal fees should Dr Bawa-Garba appeal the High Court's decision.
Doctors are fearful the case could discourage medical professionals from owning up to their mistakes, and the cultural change it could effect within the British medical system.
"One of the particularly alarming features of this case is that it seems that Dr Hadiza Bawa-Garba's reflections on her mistakes were used against her in court … in the long term that's going to be damaging to patient safety across the UK."
The GMC denies it used notes taken by Dr Bawa-Garba about that day, though accepts they may have been used in the Medical Practitioners Tribunal.
Nurse Isabel Amaro, who also treated Jack Adcock, was also convicted of manslaughter and struck off the nursing register. Dr Bawa-Garba's consultant, Dr O'Riordan, was not charged over the boy's death.
Could it happen here?
South-west Sydney paediatrician Andrew McDonald said most Australian consultant doctors would have had an experience like that of Dr Bawa-Garba's.
"Twice a week in Australia there is a serious adverse event in healthcare, child or adult. This already happens here."
Dr McDonald said the key difference was that the Australian system is better at recognising "system error".
While a similar analysis as to what went wrong would happen in Australia as in the UK, he said Australia's medical bodies are less likely to attribute blame to a particular doctor.
"It would be done by the same people, but the outcome I expect would be different. The New South Wales Medical Board or the Australian Health Practitioner Regulation Agency (AHPRA) are not perfect but I've never seen anything as vindictive and poorly informed as this."
Dr McDonald also criticised the consultant at the hospital for not going to see Jack Adcock when presented with his blood tests by Dr Bawa-Garba.
"I have no idea why he wasn't brought before the court, but before the court of his peers, consultants, to not go and see a child with a pH of 7.08 with an unexplained illness is just hopeless … this consultant has failed in his duty of care to provide safe care to this child," he said.
Chair of the Medical Board of Australia (the nearest equivalent of the UK's GMC) Dr Joanna Flynn, said a conviction of manslaughter for a doctor in Australia was incredibly rare — only "a handful of cases over perhaps 50 years".
She said it was even rarer for a conviction to be recorded against an Australian doctor.
"There is a process of open disclosure in Australia, and in fact in Victoria there is a proposal to introduce candour as a legislative requirement, which means that patients must be told if something bad has happened, why it happened, what has been learned from it, how it can be prevented," she said.
"There are protections so that explanation about what happened, and even acknowledgement that something went wrong, can't be used in litigation against the doctor in the context of an apology."
A needless death
While debate continues over the personal and systemic errors in the case, Dr Moosa Qureshi said the focus needed to be on preventing similar deaths in the future.
"But I fear that this is actually a trend rather than a glitch … these things happen all the time in medical practice and if we respond to them in this way we are really, really going to actually make things much worse because doctors are going to start feeling fearful of actually admitting mistakes."
"If that happens, then mistakes cannot be corrected and avoided in future."
Eradication of Cervical Cancer in Australia (ABC)
Text is from the ABC Australia website (health section): http://www.abc.net.au/news/2018-03-04/cervical-cancer-may-be-eliminated-in-australia-40-years-experts/9507050
Cervical cancer could be effectively eliminated in Australia within the next four decades, medical experts say, after new data revealed infection rates had plummeted to just 1 per cent in young women.
Cervical cancer could be effectively eliminated in Australia within the next four decades, medical experts say, after new data revealed infection rates had plummeted to just 1 per cent in young women.
Research published by the International Papillomavirus Society, lead by doctors in Melbourne, showed a dramatic decline in the rate of Human Papillomavirus (HPV) in women aged up to 24.
The data revealed infection had fallen from 24 per cent to just 1 per cent in that age group in the last decade.
Researchers said the decline was due to the roll-out of the national immunisation program for boys and girls, which began in 2007.
Professor Suzanne Garland, the director of the Centre for Women's Infectious Diseases at the Royal Women's Hospital, said she expected the number of cases each year would drop from about 1,000, to just a few, thanks to the vaccination and the new DNA screening test.
"That's contingent on a high coverage of vaccine. Australia is really in the lead here, [there's been] really good coverage through the school-based free vaccine program.
"For example, the genital warts the vaccine protects against, already we've seen a reduction of over 90 per cent — that's huge."
Cervical cancer is caused by HPV infection, which can lead to the growth of abnormal cells in the lining of the cervix.
About eight in 10 women are infected with HPV at some point in their lives, but most will not go on to develop cancer.
In Australia, it is estimated about 930 women will be diagnosed with the disease this year, and 258 will die.
Globally, one woman dies of cervical cancer every two minutes.
The majority of cervical cancers occur in the developing world, and Professor Garland said the effectiveness of the program in Australia proved the need to take up vaccination overseas.
"In the Pacific-Oceania and Asian region we have about half of the cases of cervical cancer in the world. We have a big job to do, but we have the tools to beat it," she said.
An improved version of the Gardasil vaccine will be available to all 12 and 13-year-olds across the country this year, while a new screening program launched in December is expected to make it easier to detect woman at risk.
Friday, 16 September 2016
I've been paid by drug companies & I've not done anything wrong
Amazing article by Dr Tom John from Melbourne. I agree with him.
I've been paid by drug companies & I've not done anything wrong
I've been paid by drug companies & I've not done anything wrong
Tuesday, 13 September 2016
Brain Surgery at McDonalds. Just fantastic!!
Medicine at its best - do the best thing for the patient, in the best way possible, in the best time possible, with the best options available.
Brain Surgery at McDonalds
Brain Surgery at McDonalds
Bought out: Sugar Industry and Heart Disease?
The article from Ars Technica goes through the gist of the conspiracy of the sugar industry paying researchers to downplay the impact of sugar and heart/coronary disease. This was decades prior to anyone knowing about the connection.
Sugar Industry bought out Researchers?
The actual article from JAMA:
Sugar Industry and Heart Disease Research: The Saga
Sugar Industry bought out Researchers?
The actual article from JAMA:
Sugar Industry and Heart Disease Research: The Saga
Saturday, 20 August 2016
Are Male Nurses discriminated against?
Great article from the ABC regarding male nurses. They work hard, struggle for their patients, are dedicated... yet are discriminated against.
Male Nurses
Male Nurses
Saturday, 13 August 2016
Largest Private Hospital in SA
Calvary has started work on the largest private hospital in South Australia. The hospital should be ready in the next few years. Massive investment. Good job.
Largest Private Hospital in SA
Largest Private Hospital in SA
Living with Cancer does not make you a Hero or a Victim
Good article in the ABC by Ranjana and Ginger about people living with cancer. We do tend to label people with cancer as heroes or as people who "deserve it".
A cancer diagnosis is sad. Full stop.
Living with cancer is not about being a hero or a victim
A cancer diagnosis is sad. Full stop.
Living with cancer is not about being a hero or a victim
Organ Transplantation in Cancer Patients
BBC article about organ donors and cancer patients. I have had several people with cancer who have pledged to donate their corneas after death. In a way they keep seeing through someone else's eyes.
Are you an Organ Donor? Worth thinking about.
http://www.bbc.com/news/health-37057933
Register to become an Organ Donor in Australia. Each country would have their own donor registry.
http://www.donatelife.gov.au
Are you an Organ Donor? Worth thinking about.
http://www.bbc.com/news/health-37057933
Register to become an Organ Donor in Australia. Each country would have their own donor registry.
http://www.donatelife.gov.au
Friday, 5 August 2016
$1000 Hospital Car Parking fine!
A mum has been hit with a $1000 car parking fine at a hospital in Perth. She brought her son (who has a congenital heart condition) to the hospital Emergency Dept and left after 2 hours. Then got a fine of a $1000.
Who decides on these rates and fines? Just amazing!
$1000 for Hospital Car Parking
Who decides on these rates and fines? Just amazing!
$1000 for Hospital Car Parking
Wednesday, 3 August 2016
Conversations about Teminal Cancer
This article in The Guardian by Dr Ranjana Srivastava is very confrontational. It delves into the possible disconnect that we as health professionals have from our patients, their families and friends.
Life is important. Dying is a part of life. Both should be taken care of.
Conversations about terminal cancer
Life is important. Dying is a part of life. Both should be taken care of.
Conversations about terminal cancer
Survivor's Wisdom
Powerful, perspective-shifting Ted Talks on what it means to live courageously. What an amazing perspective!!
An insight into people picking up the pieces of their lives and not just moving on.... just racing on.
Fantastic.
Survivor's Wisdom
An insight into people picking up the pieces of their lives and not just moving on.... just racing on.
Fantastic.
Survivor's Wisdom
How are we fighting Cancer?
Good collection of talks from the Ted playlist. Talks from researchers who've dedicated their lives and careers to understanding cancer and someday ending it.
Ted Talks - Cure for Cancer
Ted Talks - Cure for Cancer
Tuesday, 2 August 2016
Harnessing the Immune System against Cancer
The New York Times has put together a very comprehensive article discussing immunotherapy for people with cancer. Great read.
I have used these class of medication extensively and am very impressed with the results. The problem is finding the group of patients who would respond well. The quest continues.
The Immune System - NYT
I have used these class of medication extensively and am very impressed with the results. The problem is finding the group of patients who would respond well. The quest continues.
The Immune System - NYT
Evil spirits, bile and lunatic asylums: A history of insanity
A good overview of the history in treatment, punishment and diagnosis of mental illness by the ABC Health unit.
A History of Insanity
A History of Insanity
Subscribe to:
Comments (Atom)